Diabetes: Symptoms, Types, Causes, Environmental risk factors, Prevention and care
Introduction:
Diabetes mellitus is a
disease of inadequate control of blood levels of glucose. The underlying cause
of diabetes is the defective production or action in of insulin, a hormone that
controls glucose, fat and amino acid metabolism.
Characteristically, diabetes
is a long term disease with variable clinical manifestation and progression.
Chronic hyperglycemia, from whatever cause, leads to a number of
complication-cardiovascular, renal, neurological, ocular and other such as
intercurrent infection.
Sign and Symptoms of Diabetes:
 |
| Sign and symptoms of Diabetes |
Classification/Types of Diabetes:
The
classification adopted by WHO is given-
1. Diabetes
mellitus (DM)
i) Insulin
dependent diabetes mellitus (IDDM, Type-1)
ii) Non-Insulin
dependent Diabetes mellitus (NIDDM, Type 2)
iii) Malnutrition-related
diabetes mellitus (MRDM)
iv) Other type
(Secondary to pancreatic, hormonal, drug-induced, genetic and other
abnormalities)
2. Impaired glucose
tolerance (IGT)
3. Gestational
diabetes mellitus (GDM)
1. Diabetes mellitus
i) Type-1, IDDM:-
- Type 1 diabetes is also called insulin-dependent diabetes (IDDM).
- It used to be called juvenile onset diabetes, because it often in childhood.
- It is an autoimmune condition. It is caused by the body attacking its own pancreas with antibodies.
- In people with type 1 diabetes, the damaged pancreas does not make insulin.
ii) Type 2, NIDDM:-
- Type 2 diabetes is also called non-insulin dependent diabetes (NIDDM).
- The most common form of diabetes is type 2 diabetes, accounting for 95% of diabetes cases in adults.
- With type 2 diabetes, the pancreas usually produce some insulin. But either the amount produced is not enough for the body’s need or the body cells are resistant to it.
- Insulin resistance or lack of sensitivity to insulin, happens primarily in fat, liver and muscle cells.
iii) Malnutrition-related
diabetes mellitus:-
- Found mainly in developing countries due to protein deficient diabetes.
- Among 10-40 years old.
- Hyperglycemia present without ketoacidosis in malnutrition related diabetes mellitus.
- Role of malnutrition as a causal factor is unknown.
iv) Others types:-
- Secondary to pancreatic.
- Genetic and other abnormalities.
- Hormonal (insulin).
- Drug induced.
2. Impaired glucose tolerance (IGT)
Impaired
glucose tolerance (IGT) describes a states intermediate- ” at risk” group-between
diabetes mellitus and normality. It can only be defined by the oral glucose
tolerance test.
3. Gestational diabetes mellitus (GDM)
Gestational diabetes is a diabetes diagnosed for the first time during
pregnancy. Like other type of diabetes, gestational diabetes affect the cells
use sugar (glucose). Gestational diabetes cause higher blood sugar that can
affect your pregnancy and your baby’s health.
Sign and symptoms:-
Sign and
symptoms associated with gestational diabetes include:
- Increased, frequent urination
- Fatigue
- Nausea and vomiting
- Weight loss even with increased appetite
- Blurred vision
- Yeast infection
Risk factor:-
Risk
factor of gestational diabetes are as follows:
- Being overweight
- Having an immediate family member with diabetes
- Having polycystic ovary syndrome
- Not being physically active
- Having prediabetes
Causes:-
Gestational
diabetes is a form of diabetes that occurs during pregnancy. It is
characterized by high blood sugar levels and typically resolves after
childbirth. The exact causes of gestational diabetes are not fully understood,
but several factors are believed to contribute to its development.
Here are
some of the potential causes:
- Hormonal changes
- Genetic predisposition
- Obesity or excessive weight gain
- Age, ethnicity
- Previous history of gestational diabetes
- Polycystic ovary syndrome (PCOS)
It is
important to note that gestational diabetes can occur even in women without any
of these risk factors. Regular prenatal check-ups, including glucose screening
tests, are crucial to diagnose and manage gestational diabetes effectively. A
healthcare provider can provide personalized advice and guidance based on an
individual’s specific situation.
Prevention:-
While there
is no guaranteed way to prevent gestational diabetes, there are steps you can
take to reduce your risk. Here are some strategies that may help in preventing or minimizing
the risk of gestational diabetes:
- Eat a balanced diet
- Maintain a healthy weight
- Be physically active
- Monitor carbohydrate intake
- Stay hydrated
- Regular prenatal care
- Manage stress
- Start pregnancy at a healthy weight
- Don’t gain more weight
Remember,
even with the best preventive measures, some women may still develop
gestational diabetes. Regular prenatal check-ups and screenings are essential
to detect and manage the condition effectively. If you have specific concerns
or risk factors, it’s important to consult with your healthcare provider for
personalized guidance.
Environmental
risk factor of Diabetes:
Susceptibility
to diabetes appears to be unmasked by a number of environmental factor acting
on genetically susceptible individuals.
They
include-
i)
Sedentary life style:- Sedentary life style appears to be an important risk factor for
the development of NIDDM. Lack of exercise may after the interaction between
insulin and its receptors and subsequently lead to an NIDDM.
ii)
Diet:- A high saturated fat intake has been associated with a higher
risk of impaired glucose tolerance, and higher fasting glucose and insulin
levels.
iii)
Dietary fibre:- In many controlled experimental studies, high intakes of dietary
fibre have been shown to result in reduced blood glucose and insulin levels in
people with type 2 diabetes and impaired glucose tolerance.
iv)
Malnutrition:- Malnutrition is really infancy and childhood may result in
partial failure of beta cell function. Damage to beta cells may explain the
associated impaired carbohydrate tolerance in kwashiorkor.
v)
Alcohol:- Excessive intake of alcohol can increase the risks of diabetes
by damaging the pancreas and liver and by promoting obesity.
vi) Viral
infection:- Among the viruses that have been implicated are rubella, mumps
and human coxsackie virus B4. Virus infection may trigger an immunogenetically
suspectible people a sequence of events resulting in beta cell destruction.
vii)
Chemical agent:- A number of chemical agents are known to be toxic to beta cells,
e.g., alloxan, Streptozotocin, the rodenticide VALCOR etc. A high intake of
cyanide producing foods may also have toxin effect on beta cell.
viii)
Stress:- Surgery, trauma and trace of situations, internal or external,
may “bring out” the disease.
ix) Other
factors:- High and low rates of diabetes have been linked to a number of
social factors such as occupation, marital status, religion, economic status,
education and changes in lifestyle which are element of what is broadly known
as social class.
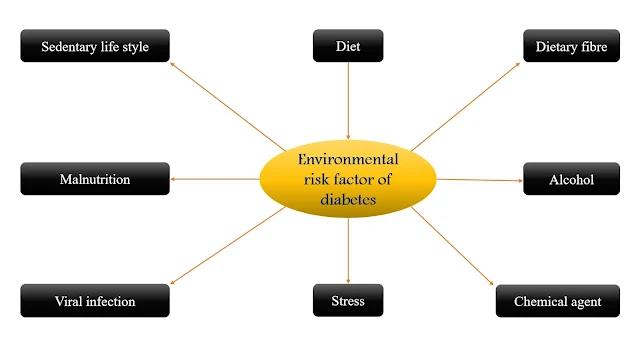 |
| Environmental risk factor of Diabetes |
Prevention and
care of Diabetes:
1. Primary prevention:-
Two
strategies for primary prevention have been suggested:
i)
Population strategy:-
The scope
for primary prevention of IDDM is limited on the basis of current knowledge.
However, the development of prevention programs for NIDDM based on elimination
of environmental risk factor is possible. The preventive measure comprise
maintenance of normal body weight through adoption of healthy nutritional
habits and physical exercise.
ii) High
risk strategy:-
There is no
special high risk strategy for IDDM diabetes. Since, NIDDM appears to be linked
with sedentary lifestyle, over nutrition and obesity, correction of the risks
of diabetes and its complication. Since alcohol can indirectly increase the
risks of diabetes, it should be avoided.
2. Secondary prevention:-
When
diabetes is detected, it must be adequately treated.
The aims
of treatment are-
a) To
maintain blood glucose levels
b) To
maintain ideal body weight.
- Diet alone.
- Diet and antidiabetic drug.
- Diet and insulin.
i)
Glycosylated hemoglobin:-
There
should be an estimation of glycosylated hemoglobin of half-years of intervals.
The test provides a long-term index of glucose control.
ii)
Self-care:-
The
diabetic should take a major responsibilities for his own healthcare with
medicine guidance- e.g., examination of his own urine and where possible blood
glucose monitoring, maintenance of optimum weight, decrease of intake, alcohol.
The patient should carry an identification card showing his name, address,
telephone number and details of the treatment he is receiving. In short, he
must be a working knowledge of diabetes. All these mean education of patients
and their families to optimize the effectiveness of primary care.
3. Tertiary prevention:-
Diabetes is major cause of disabilities through its
complication, e.g., blindness, kidney failure, coronary thrombosis etc. The
main objective at the tertiary level is to organize specialized clinics. This
is a great need to establish such clinics in large town and cities.
